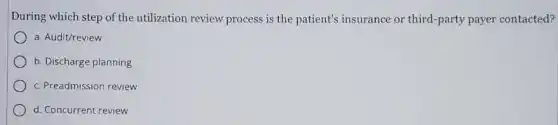
During which step of the utilization review process is the patient's insurance or third-party payer contacted? a. Audit/review b. Discharge planning c. Preadmission review d. Concurrent review
Solution4.0(245 votes)
Answer
Explanation
Similar Questions
Both absolute comparisons and relative comparisons are methods for identifying decision criteria. Select one: True False
Which of the following is TRUE of the Right of Recovery condition of the Inland Marine policy? The policyholder must not hamper the right of the insurer to recover damages from a third party. The insurer must not hamper the right of the policyholder to recover damages from a third party. Rights of recovery only apply to potential future losses. The insured and the insurer have equal rights to recovery of property.
Which of the following would be a valid I reason why a policy premium would be higher than the standard premium? A. The insured does not have the necessary financial reserves B. The insured does not meet established underwriting requirements C. The agent quoted the wrong price D. The insurer is not a member of the MIB
Fill in the blank with the correct term. __ is the amount charged by a lender for borrowing money. Answer Interest Principal Interest rate Annual percentage rate
Suppose the demand for rescue services in our national parks is perfectly inelastic. This fact would mean that a 31 percent increase in rescue fees leads to A no change in the quantity demanded. B a 31 percent increase in demand. C a decrease in the quantity demanded to 0 rescues. D a 31 percent decrease in demand. E a 31 percent decrease in the quantity demanded.
As the length of your investment horizon increases, you can assume greater risks with your investing. True False
When a bank deducts any amount other than a paid check from a depositor's account, it issues a form called a(n):
Multiple Choice Question Which statement is true about marketing channels? More intermediaries are involved in direct channels. Every channel must have a retailer in it. Indirect channels are longer than direct ones. Every channel must have an agent in it.
Which of the following does a life insurance policy summary normally include? A. O Stated beneficiary B. Agent's report C. The policy's cash value D. Policyowner's MIB report
10. What happens if the score reaches $20-20$ ? a) Game ends b) Continue until one player leads by 2 c) Play a tiebreaker d) Restart the game









